
We often hear about the burden of depression in adulthood but depression can and does affect young people. While depression is less likely to affect young children, an adolescent is just as likely as an adult to experience an episode of depression in a year, with a 12-month prevalence rate of 4-5% (Thapar et al., 2012).
Depression in children and adolescents is associated with a higher risk of self-harm, suicide, other mental health problems, as well as social and educational difficulties and disadvantage. Those who experience depressive symptoms in childhood or adolescence are at greater risk of grappling with the disorder in adulthood.
The good news is that treatments are available but ideally we want to prevent young people from experiencing depression in the first place. Brunwasser & Garber’s 2015 review aimed to establish whether there is evidence to support the implementation and dissemination of programs to prevent childhood and adolescent depression. Thus, the review’s overall aim was not merely to determine whether there are programs that work for preventing depression, but to assess how ready these are to be widely disseminated.
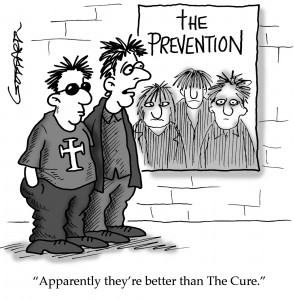
Prevention is important!!
Methods
This is a systematic review, which means that the authors systematically gathered data from previously published studies to summarise, evaluate and draw conclusions based on a broad evidence base.
The authors were very strict in their inclusion criteria. Following the Society for Prevention Research – Standards of Evidence guide (SPR-SOE), they only reviewed prevention programs that were evaluated in at least two studies, which:
- Randomly allocated participants to a prevention program.
- Compared the outcomes of the prevention program to those of a realistic, naturally occuring control group, such as a waiting list group or a group experiencing usual care. Studies that did not include any form of natural control group but instead compared the intervention to an active control group, such as another intervention or a placebo group, were excluded.
- Measured depressive symptoms explicitly. Studies that measured related constructs, such as positive emotions, were not included.
- Were published in an English-language and peer-reviewed journal.
- Mostly included children or adolescents under the age of 18.
- Examined explicit prevention programs. If a study called their program a “treatment” or if it tested it among people who were depressed at the time of the intervention, it would be excluded.
The authors searched the PsycINFO database only and found 614 studies, of these 37 were included. These studies evaluated 11 different prevention programs.
Results
The majority of prevention programs were delivered in schools and most of them were based on cognitive-behavioural principles. Most of the programs catered for children who were between 9-11 years old.
The first criterion for the authors was the efficacy of the programs. Efficacy is an indicator of how well the program works under ideal and controlled circumstances. In an ideal world (with enough funding, ideal participants and conducted by enthusiastic researchers), does the program prevent depression?
- The majority of programs prevented depressive symptoms. For example, 8 out of the 11 programs achieved better outcomes than a control group, across several randomised controlled trials. 5 of these prevented symptoms for over a year after the program ended.
- When it came to depressive episodes as an outcome (rather than symptoms), only two programs were supported by strong evidence.
The second criterion was effectiveness. This is an indicator of how the program fares under more real-world conditions, for example when teachers (rather than researchers) deliver the program, or when it is conducted independently of the program developers.
- 6 out of the 11 programs did well when they were delivered by real-world group leaders, such as teachers or clinicians.
- 3 programs were found to be effective in studies conducted independently of the program developers (but two of those did not have any sustained effects).
- There were very few studies where the program was delivered by clinicians or teachers AND also evaluated independently of the program developers, and none of these demonstrated better outcomes.

The majority of programs prevented depressive symptoms: 8 out of the 11 programs achieved better outcomes than a control group.
Conclusion
According to the authors “No youth depression prevention program has yet garnered sufficient evidence of effectiveness under realistic conditions to warrant widespread dissemination at this time”.
The key word here is “yet”. There were some promising candidates among the programs, which showed relatively consistent positive effects, but need to be evaluated under more realistic conditions, such as the “Coping with Stress Course”, the “Blues Group” program and the “Interpersonal Psychotherapy-Adolescents Skills Training (IPT-AST)”. Thus, at this point, the problem is not necessarily the lack of promising programs to prevent depression, but the lack (and the quality) of studies evaluating their effectiveness.
The authors also highlight some additional questions that future studies of depression prevention programs should take into account, to close the gap between finding that a program is efficacious, and implementing it widely. Some of these are:
- Several programs had beneficial effects immediately after the program ended, but they did not last longer than a few months. From a public health point of view, is this enough to make their implementation worthwhile?
- What is a meaningful reduction in depressive symptoms? For example, does a statistically significant reduction of depressive symptoms translate into a noticeable difference for children and youth?
- Should there be a wider move towards assessing functional outcomes, such as school absence, in addition to prevention of symptoms or diagnoses, to establish the practical significance of an effective program?

Better effectiveness studies are one of the missing links between demonstrating an effect and implementing the program.
Summary
This is a very comprehensive review of prevention programs on depression. Overall it is great to see a summary analysis that not only looks at whether programs work, but specifically focuses on whether they work under realistic conditions and are “fit for practice” because ultimately, this is the expectation that any intervention has to live up to.
The conclusion that the authors drew appears to be justified on the basis of the research they review and the guidelines they use, although some of these could be questioned – for example, it is unfortunate that the authors only included studies published in English-language journals, as it meant that German-language studies on one of the programs, “LARS&LISA” had to be excluded. In this day and age, language should not be a barrier. It is also not clear why the authors restricted themselves to searching articles only via one database (PsycINFO). In addition, as the authors themselves discuss, some of the guidelines are vague as to what constitutes a positive public health impact; developing these further will play its part in bridging the gap between effectiveness and implementation.
Links
Primary link
Brunwasser, S. M., & Garber, J. (2015). Programs for the Prevention of Youth Depression: Evaluation of Efficacy, Effectiveness, and Readiness for Dissemination. Journal of Clinical Child & Adolescent Psychology, 1–21. doi:10.1080/15374416.2015.1020541 [Abstract]
Other references
Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. doi:10.1016/S0140-6736(11)60871-4 [Abstract]
National institute of mental health fact sheet on depression in children and adolescents
http://www.nimh.nih.gov/health/publications/depression-in-children-and-adolescents/index.shtml